The Science Behind Rapid Antigen Tests: How Reliable Are They?
Rapid antigen tests have become a crucial tool in the fight against infectious diseases, particularly during the ongoing COVID-19 pandemic. These tests, also known as rapid diagnostic tests (RDTs), are designed to quickly detect specific viral proteins in a patient’s sample, providing rapid results within minutes.
While they offer undeniable advantages in terms of speed and accessibility, questions have arisen about their reliability and accuracy. To truly understand the science behind rapid antigen tests and their reliability, we must delve into their design, mechanism of action, and factors that influence their accuracy.
Design and Mechanism
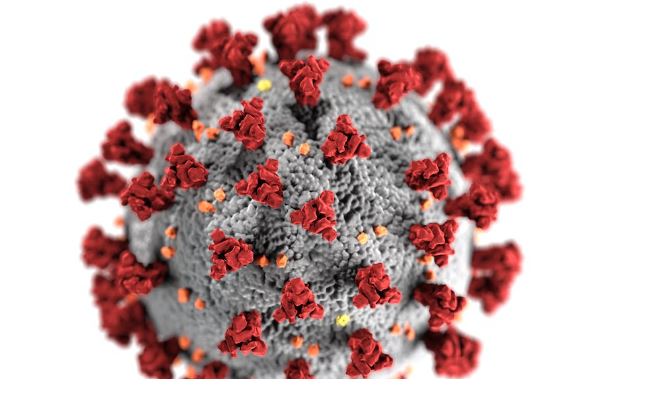
Rapid antigen tests are based on the principles of immunochromatography, a technique that exploits the interaction between antigens and antibodies. In the case of COVID-19, the target antigen is typically the spike protein found on the surface of the SARS-CoV-2 virus.
The test device consists of a strip or card with specific zones containing antibodies. The sample, usually obtained from a nasal or throat swab, is applied to the strip. If the target antigen is present in the sample, it binds to the antibodies on the strip, forming a visible line.
The simplicity of this mechanism allows for rapid results, making rapid antigen tests a valuable tool for mass screenings and immediate decision-making, such as at airports, schools, and healthcare facilities. If you’re planning to get tested, it might be a good idea to order lateral flow tests.
Factors Influencing Reliability
The reliability of rapid antigen tests depends on several factors:
Viral Load
Rapid antigen tests are generally most reliable when a person has a high viral load, meaning there is a substantial amount of virus present in their sample. During the early stages of infection or in asymptomatic individuals with lower viral loads, the sensitivity of these tests may decrease, leading to false-negative results.
Specificity and Sensitivity
The terms “specificity” and “sensitivity” are crucial indicators of a test’s reliability. Specificity refers to a test’s ability to correctly identify those without the disease, while sensitivity indicates its ability to correctly detect the disease in those who have it. Rapid antigen tests tend to have high specificity, meaning they are good at correctly identifying negative cases. However, their sensitivity can vary, and false negatives can occur.
Mutation Variants
The ongoing evolution of viruses, like SARS-CoV-2, can impact the performance of rapid antigen tests. If the target antigen mutates significantly, the antibodies on the test strip might not bind as effectively, potentially leading to false-negative results.
User Error
Proper sample collection and handling are critical for accurate results. Incorrect swabbing techniques or mishandling of the test kit can lead to unreliable outcomes.
Timing
The timing of the test in relation to symptom onset can affect its accuracy. Rapid antigen tests might perform better when administered during the symptomatic phase of the illness.
Advantages and Use Cases
Rapid antigen tests offer numerous advantages:
Speed
Results are available within 15-30 minutes, enabling quick decision-making and isolation measures.
Accessibility
These tests are relatively inexpensive and do not require specialized laboratory equipment.
Mass Screening
Rapid antigen tests are well-suited for mass screenings in high-risk settings, contributing to disease containment efforts.
Early Detection
Despite potential limitations, rapid antigen tests can still detect contagious individuals early in their infection, helping to break the chain of transmission.
The reliability of rapid antigen tests is influenced by a complex interplay of factors, including viral load, test sensitivity, mutation variants, user technique, and timing. While they may not be as sensitive as PCR tests, which detect viral genetic material, rapid antigen tests provide a valuable tool for quick and widespread screening, especially in situations where immediate results are crucial.
These tests have played a significant role in managing the COVID-19 pandemic and will likely continue to be an essential component of public health strategies in future infectious disease outbreaks. As with any diagnostic tool, understanding their strengths and limitations is key to their effective and responsible use.